- At the clinic's price without markups
- with full doctor support
What is a bone marrow transplant?
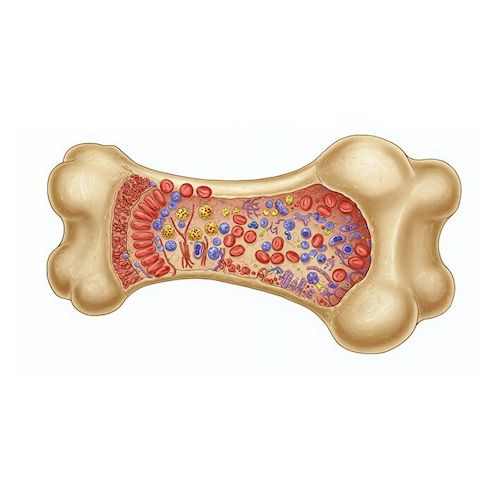
A bone marrow transplant (abbreviated BMT) is an intravenous infusion to renew hematopoietic stem cells (HSC). The procedure involves replacing the patient's dysfunctional bone marrow with healthy bone marrow (either your own or donor's). To understand the importance of such an operation, it is first worth understanding what bone marrow (BMЕ) is and what makes it unique.
What is important to know about bone marrow and the hematopoietic system for people with hematological and immune diseases
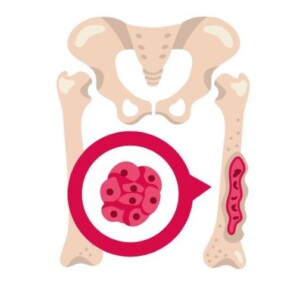
Red bone marrow is the main part of the hematopoietic system, namely the organ that is found in flat and tubular bones. It is a spongy tissue that produces ALL the elements of the blood. This process has a beautiful name "hematopoiesis". When a doctor suspects that something is wrong with a patient's health, he most often evaluates the volume of these cells in laboratory tests:
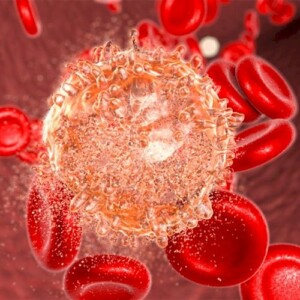
- leukocytes or white blood cells, which act as defenders against fungi, viruses, and bacteria;
- thrombocytes or platelets, which promote blood clotting and participate in the restoration of damaged vessels.
In addition to these blood elements, other elements (for example, hemoglobin) are also present in the tests. Therefore, it is with a complete blood count that one can draw conclusions. Is the body fighting an infection, are there signs of a serious hematological disease, and so on? In some cases, blood tests can even indicate cancer. But let's return to the bone marrow.
BM cells provide constant blood renewal and support vital functions. But not everyone knows that numerous “specialists” also come from hematopoietic stem cells, some of which have special properties in the fight against serious diseases.
What other blood elements resist infections?
Dendritic cells are the “scouts” and “teachers” of our immunity. They also come from the bone marrow and constantly patrol the body, especially in places of contact with the outside world (skin and mucous membranes). Their unique ability is to detect samples of any suspicious “foreigners” (viruses, bacteria, tumor particles), and then present them to T-lymphocytes. It’s like showing a sketch of a criminal to detectives: dendritic cells teach T-lymphocytes exactly who to look for and destroy. Thanks to this, they launch a powerful and accurate immune response.
It is interesting that this is the property that scientists use to develop dendritic cell vaccines. They train the patient’s immunity to fight malignant tumors. This treatment technology is used in the best clinics in Germany, Turkey and Israel.
T-lymphocytes (or T-cells) are practically the “special forces” of the immune system. They also originate in the BM. Their main task is the targeted destruction of atypical cells, viral and bacterial agents. In a normal state of human health, a T-lymphocyte detects a suspicious agent, immediately eliminates it, preventing the spread of infection or tumor growth.
In modern medicine, they have learned to modify T-cells (CAR-T-cell therapy) so that they more effectively find and destroy cancer, giving hope to people with severe forms of lymphoma or leukemia.
What is the hematopoietic system as a whole?
In addition to the bone marrow (the main “blood factory”), our body also has other organs that everyone has heard of, but does not fully understand their functions. They work to protect and renew the blood and immunity together:
- Spleen is a kind of “filter” in the human body. This organ cleanses the blood of old or damaged cells, thus helping to fight infections.
- Lymph nodes are “checkpoints” throughout the body. They filter lymph (the fluid that washes the body’s tissues) and are the place where immune cells meet viruses and bacteria to mount an attack.
- Thymus gland is an organ located behind the breastbone. It is like a “school” for special immune cells – T-lymphocytes. This is where they learn to distinguish foreign microorganisms so as not to attack their own good cells.
Conclusions: these organs, together with the red bone marrow, form a complex hematopoietic system so that we are healthy and protected from various types of infections.

Saving bone marrow is an absolute priority
The BMT procedure is critically important since it allows to completely replace the bone marrow affected by the disease with adequately functioning one. Transplantation may be the only way to restore the hematopoietic system, ensuring the production of all the blood cells necessary for survival. Without this new start, all the body's systems fail, and the patient will not be able to recover.
Which clinic to choose?
Which clinic to choose?
For the treatment of severe hematological diseases, you can consider several options for clinics abroad.
You can find out the exact cost of transplant operations from a related or unrelated donor from the coordinator-doctor by leaving a request on this page. The hospitals listed below offer additional methods of fighting cancer that are used in the best clinics in the world.
Samsung Medical Center (Seoul, South Korea)
Samsung is one of the leading medical centers in Asia, known for its innovations, research, and high success rates in cancer treatment. Here, patients have access to CAR-T cell therapy. This is a new method in which the patient's own T-lymphocytes are modified to recognize and destroy cancer cells. This is especially promising for the treatment of refractory leukemia and lymphoma. An approach based on genomic analysis of the patient's tumor (Tgen) is actively used to create individual treatment plans. Samsung has a powerful research base that allows not only to effectively implement but also to improve bone marrow transplant procedures.
Medical Park Hospitals (Antalya, Istanbul, Turkey)
Medical Park is one of the largest network hospitals in Turkey. They are known worldwide for their organ and bone marrow transplant centers. They emphasize compliance with international protocols and standards (for example, EBMT – European Society for Blood and Marrow Transplantation). Specialized adult and pediatric bone marrow transplant centers are integrated into international donor bone marrow banks.
High-tech diagnostics and therapy of oncopathologies include the use of PET-CT machines for staging, monitoring, and assessing the response to treatment in lymphomas, myeloma, and some types of leukemia. Related and unrelated donor transplants, as well as haploidentical bone marrow transplants are performed here.
Centro Médico Teknon (Barcelona, Spain)
Teknon is part of the Quirónsalud Hospital Group, known for its specialized treatments and advanced technologies. They use a multidisciplinary approach to the treatment of cancer patients, bringing together specialists in hematology, oncology, radiology, and other fields. Here, patients have access to molecular and genetic diagnostics. This is a detailed analysis of genetic mutations in blood cells and bone marrow to accurately determine the type of leukemia, lymphoma or myeloma, as well as predict the response to treatment. Teknon performs Flow Cytometry, a highly sensitive method for detecting minimal residual disease, which is key to monitoring remission.
Teknon offers Haploidentical BMT, a transplant method when a complete HLA-compatible donor is not available. It allows the use of a parent, child or other relative as a donor who is only 50% compatible. In the clinic, this technique is used with post-transplant cyclophosphamide to reduce the risk of bone marrow rejection. This drug is usually administered 3-4 days after the HSC transplant. Reduced intensity conditioning BMT (RIC BMT) allows transplants to be performed in elderly patients who are not suitable for high-dose chemotherapy.
Ichilov (Tel Aviv, Israel)
Sourasky Medical Center (formerly Ichilov) is one of the world's leading centers for bone marrow transplantation. The clinic has introduced advanced technologies and innovative approaches to the treatment of hematological diseases. It performs both autologous and allogeneic transplants for adults and children. Ichilov has a specialized institute, which provides unique opportunities for a full cycle of cell therapy.
Ichilov was one of the first hospitals to introduce the revolutionary CAR T-cell therapy technology for the treatment of blood cancer. Complex hematological research and diagnostics are also performed here. Modern chemotherapy protocols, targeted and biological therapy, as well as advanced antibacterial, antifungal and antiviral drugs to combat infectious complications are used in Sourasky Hospital.
What are the main stages of the BMT process?
Bone marrow transplantation is a structured process that usually consists of several key stages. It begins long before the transplant itself and continues long after the surgery.
Stages of bone marrow transplantation:
What is important to know about a bone marrow donor
To become a bone marrow donor, a person must be absolutely healthy and meet strict medical criteria. This is important to know not only for the candidates themselves but also for relatives who choose a donor for the patient from their family.
Age of the donor for HSC transplantation
The optimal age is 18-35 years (maximum up to 45). This ensures better cell engraftment and lower risks for the donor and recipient. Some registries allow registration up to 60 years, but older people are less often selected for this mission.
General health
Oncological diseases, HIV, hepatitis B and C, tuberculosis; serious pathologies of internal organs – heart, lungs, kidneys, and liver are unacceptable. People with autoimmune diseases (for example, multiple sclerosis, systemic lupus erythematosus) cannot participate as bone marrow donors. Serious mental disorders are excluded.
Time restrictions for potential donors, pregnancy, and breastfeeding
Weight must be at least 50 kg. There are also restrictions on the body mass index (BMI) to prevent risks associated with obesity or exhaustion.
Histocompatibility (HLA typing) is the most important criterion. The donor must be maximally compatible with the recipient by genetic markers, which is determined by a special blood test.
Is it possible to ask a child to become a bone marrow donor for brothers and sisters?

According to the ethical guidelines and practices of leading medical organizations (for example, the American Academy of Pediatrics), donation from children is acceptable under certain conditions.
Although 50 kg is the standard minimum for adult donors and for children the specific weight indicator may be less. It always depends on the age of the child, his or her general health, and the volume of cells needed for the recipient. Doctors strive to collect a sufficient number of stem cells without exposing the donor to undue risk. In very young children (even less than 6 kg), it is possible to collect peripheral blood cells (apheresis) but this requires special equipment and the experience of the medical team.
What are the different types of bone marrow transplants?
What are the different types of bone marrow transplants?
Bone marrow transplant is not a single universal procedure but several different approaches that are chosen based on the severity of the patient's condition and diagnosis. The main difference is where the healthy HCTs come from.
Who decides what type of BMT is needed in each specific case?
The type of bone marrow transplant and its timing is determined by a team of highly qualified doctors. This is not the decision of one doctor, but a group of specialists:
- a hematologist-transplantologist is the main doctor specializing in blood diseases and directly performing BMT;
- an oncologist, if the patient's disease is associated with cancer;
- immunologists assess the state of immunity and risks;
- pathologists and geneticists provide accurate information about the type and stage of the disease.
The timing of the procedure will depend on the patient's condition and the availability of a donor. In aggressive forms of blood cancer or severe aplastic anemia, a transplant may be needed as soon as possible. While in other cases a more thorough donor search and recipient preparation may be necessary.
Autologous Bone Marrow Transplant
The prefix “Auto” means “own.” In this case, the patient is both the donor and the recipient. The patient’s own stem cells are collected before intensive chemotherapy (conditioning) begins. These cells are frozen and stored. After the patient undergoes preliminary treatment that destroys diseased cells (including his own bone marrow), his previously collected and thawed stem cells are returned to him.
When is autologous BMT sufficient? When is autologous BMT sufficient? This method is often used for certain types of lymphoma (cancer of the lymphatic system) and multiple myeloma (cancer of plasma cells), as well as neuroblastoma and other aggressive forms of cancer. It allows for strong chemotherapy that would be fatal without bone marrow support. There is no risk of rejection because the transplanted cells are native to the body.
Autologous Bone Marrow Transplant
The prefix “Auto” means “oneself.” In this case, the patient is both the donor and the recipient. The patient’s own stem cells are collected before intensive chemotherapy (conditioning). These cells are frozen and stored. After the patient undergoes preliminary treatment that destroys diseased cells (including his own bone marrow), his previously collected and thawed stem cells are returned to him.
When is autologous BMT sufficient? This method is often used for certain types of lymphoma (cancer of the lymphatic system) and multiple myeloma (cancer of plasma cells), as well as for neuroblastoma and other aggressive forms of cancer. It allows for strong chemotherapy that would be fatal without bone marrow support. There is no risk of rejection, because the transplanted cells are native to the body.
Allogeneic Bone Marrow Transplant
The prefix “Allo” means “other.” In this type of BMT, the patient receives stem cells from another person. The donor must be as compatible as possible with the recipient for certain genetic markers (HLA antigens). This is necessary to eliminate the risk of complete rejection or the development of a serious complication - the condition of "graft versus host" (when the transplanted cells attack the patient's body). A relative can become a donor, as well as a suitable volunteer from a special world registry. There are Turkish and European bone marrow donor banks.
When is an allogeneic transplant advisable? This method will be the main one for the treatment of leukemia, aplastic anemia, some hereditary blood and immune diseases. The advantage of an allogeneic transplant is not only the replacement of diseased bone marrow, but also the effect of "graft versus malignant tumor". This means that the transplanted donor HSCs will help destroy the patient's residual atypical cells.
Haploidentical Bone Marrow Transplant
This is a type of allogeneic transplant, but with one important difference: the donor is partially compatible with the recipient. Usually, this is one of the patient's parents or children, because they always have at least 50% genetic compatibility. Previously, such BMTs were very risky, but thanks to modern methods of preparation and treatment after the operation (for example, special drugs that control the immune response), they have become safer and more effective.
For what cases is haploidentical BMT suitable? Bone marrow transplant from a partially compatible donor is a life-saving option when it is impossible to find a fully compatible person (neither among relatives nor in registries). This significantly expands the circle of patients who can receive a life-saving transplant, especially for those with rare genetic types.
Complications and side effects management
Side effects after bone marrow transplantation are mainly due to the intensive preparatory therapy, which completely destroys diseased cells, but also healthy ones, and therefore strongly suppresses the immune system.
Effects on breathing
The treatment can damage lung cells, and a weakened immune system makes the body vulnerable to respiratory tract infections. This can lead to shortness of breath, weakness of the respiratory muscles, and decreased lung function. Rehabilitation, including breathing exercises and exercise machines, helps to restore their function and prevent complications.
Effects on the musculoskeletal system
Air conditioning, prolonged bed rest, general intoxication of the body and loss of appetite lead to a significant loss of muscle mass and strength (atrophy). Patients experience weakness, difficulty walking, and loss of coordination.
What are the possible indications for stem cell transplantation?
According to the recommendations of the European Society for Blood and Marrow Transplantation (EBMT) and the American Society for Transplantation and Cellular Therapy (ASTCT), BMT is indicated for the following diagnoses.
• myeloid leukemia, it occurs often after the first or second remission, to prevent relapses; • lymphoblastic leukemia, usually in the first remission for patients with a high risk of relapse or after the first relapse. • non-Hodgkin’s lymphomas, especially aggressive forms (eg, diffuse large B-cell lymphoma), in relapse or refractory forms, often as autologous BMT; • Hodgkin’s lymphoma, in relapse or refractory forms, mainly autologous BMT. • mainly as part of initial treatment for patients eligible for BMT, usually autologous transplant. • for patients at high risk of progression to leukemia. • high-risk myelofibrosis that may progress to leukemia. • aplastic anemia, if there is no response to immunosuppressive therapy or it is for patients for whom it is the first line of choice; • thalassemia, sickle cell anemia, more often in young patients for complete cure; • congenital and other primary immunodeficiencies; • hereditary metabolic diseases (adrenoleukodystrophy, mucopolysaccharidosis). • not often, but BMT can be used for certain aggressive forms, such as germ cell tumors, breast cancer (in certain clinical trials). This is usually an autologous transplant after high-dose chemotherapy.BMT is indicated for the following diagnoses:
Is BMT suitable not only for the treatment of oncohematological diseases?
According to the NMDP (formerly the National Marrow Donor Program®), one of the most well-known immune deficiencies treatable with BMT is combined immunodeficiency (SCID). This is a disease in which the body has virtually no functional T and B lymphocytes, making it extremely vulnerable to any infection. In this case, donor bone marrow is the only treatment for SCID that allows for full restoration of health.
Contraindications to Hematopoietic Stem Cell Transplantation (HSCT)
- Severe, uncontrolled problems with internal organs. A transplant cannot be performed if a person has irreversible damage to the heart, lungs, kidneys, or liver that will not allow him to withstand intensive treatment.
- Active, uncontrolled infection. The presence of a serious infection that cannot be cured + powerful chemotherapy completely suppresses the immune system, which can lead to fatal complications as a result.
- Progression of cancer that does not respond to treatment. If the tumor is actively growing and remission cannot be achieved before transplantation, the procedure may be ineffective.
What is important to know about HSC transplantation in elderly patients?
According to Moffitt Cancer Center, which has become one of the leading cancer centers in the United States, the upper age limit for BMT was previously about 65 years. This was due to the fact that intensive chemotherapy before transplantation, as well as the procedure itself, create a significant burden on the body. Older people tolerated them more severely, having a higher risk of serious complications and mortality.
Thanks to the development of medicine, in particular the emergence of reduced-intensity conditioning (RIC) protocols, it has become possible to perform transplants on older patients. These protocols are less toxic, allowing people with underlying medical conditions or at an older age to undergo HSC transplantation.
Bone Marrow Transplant Rehabilitation
The main goal of BMT rehabilitation is to restore physical fitness and psychological health. Leading clinics around the world, including those located in Turkey, South Korea, Germany, and Spain, use multifaceted approaches tailored to the needs of each patient.
BMT rehabilitation is aimed at overcoming fatigue, muscle weakness, functional limitations, psychological problems, as well as restoring cardiovascular and pulmonary function.
Physical Therapy and Kinesitherapy (Motor Function Restoration)
Early therapeutic exercise includes practice from passive movements in bed to active exercises, walking, and exercise bikes. The focus is on strengthening muscles, improving balance and coordination.
Robotic rehabilitation involves the use of special equipment to intensify training and improve the accuracy of movements. It is especially effective in cases of severe weakness or neurological complications. Exoskeletons (e.g. Lokomat, ReWalk) can be useful for gait rehabilitation. They allow patients with severe weakness or even paralysis of the legs to practice gait patterns. Robotic upper limb systems (Armeo, Amadeo) are used to train fine motor skills, strength and coordination of the hands and fingers.
Respiratory rehabilitation (pulmonary rehabilitation)
It is important for patients with complications, such as pulmonary fibrosis and infections. Exercises include diaphragmatic breathing, breathing with resistance, and airway clearance techniques. Spirometers are used to improve lung function, breathing trainers with resistance (e.g. PowerBreathe) to strengthen the respiratory muscles. PEP devices and Flutterу are used to cough up sputum.

Individual nutrition plans created by nutritionists may include special protein mixtures, vitamin and mineral complexes. In some cases, parenteral (intravenous) or enteral (through a tube) feeding. To control the nutritional status, patients undergo body monitoring (bioimpedance analysis) using special laboratory equipment.
Long-term monitoring and management of complications
People after BMT are recommended to undergo regular examinations to detect late complications (bone problems or the occurrence of secondary tumors). For this, a densitometer is used, which evaluates bone density (prevention of osteoporosis caused by steroids). Doctors use highly sensitive imaging devices (PET-CT, MRI 3 Tesla) for early detection of relapses.
Success in the treatment of oncohematological diseases depends not only on the correct selection of a donor for BMT and the quality of the procedure. Modern diagnostic methods and additional therapy play an important role. For example, CAR T-cell, targeted and immunotherapy combined with comprehensive rehabilitation programs are medically proven. Turning to leading global clinics increases the chances of recovery due to access to the best protocols and individual care.
Sources:
- https://www.immunodeficiencyuk.org/immunodeficiency/treatment/bonemarrowtransplantation/
- https://www.nmdp.org/patients/understanding-transplant/diseases-treated-by-transplant/severe-combined-immunodeficiency
- https://www.cancer.gov/about-cancer/treatment/types/stem-cell-transplant
- https://www.moffitt.org/treatments/blood-bone-marrow-transplant/blood-bone-marrow-transplant-faqs/