At each stage of the examination, the doctor receives all the necessary data for making a diagnosis: the stage of the lymphoma, the prevalence of the oncological process in the body, and the state of other organs and body systems against the background of cancer. The sequence of procedures may differ in different Israeli hospitals but the principles of research and the benefits of them remain unchanged.
Typically, diagnosis includes the following procedures:
- Biopsy
Depending on the medical condition, doctors may perform a biopsy in a variety of ways.
 Bone marrow aspiration
Bone marrow aspiration
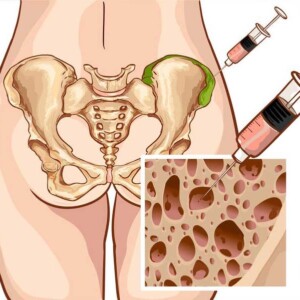
A bone marrow aspiration biopsy is the second most important diagnostic procedure. It is necessary to examine the cellular composition of the bone marrow to determine whether it is affected by tumorigenesis. The larger the sample, the more tissue the pathologist can examine, which increases the accuracy of the diagnosis.
During this procedure, the surgeon makes an incision to remove the entire lymph node (excisional biopsy) or most of the tissue (incisional biopsy).
If the lymph node is located close to the surface of the skin, the procedure can be performed under local anesthesia to numb the area. If the lymph node is in the chest or abdomen, the patient is sedated and the surgeon removes the tissue either laparoscopically (through a tube inserted into the abdomen) or through abdominal surgery.
Needle biopsy
This procedure is used when the lymph nodes are located deep in the chest, abdomen, or in other places that are difficult to access for the excisional tissue sampling method. In some cases, there may be medical reasons to avoid excisional or incisional biopsy.
During this procedure, a special needle is inserted into a lymph node having cancer, and a small sample of tissue is removed. The needle biopsy of the lymph node can be performed under local anesthesia.
Bone marrow aspiration
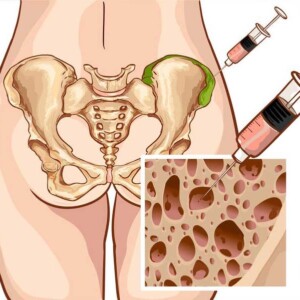
Bone marrow biopsy with aspiration is not used for initial diagnosis. An aspiration biopsy is needed to collect bone marrow for analysis before a stem cell transplant or for chromosome analysis. Bone marrow is a spongy, soft substance found inside bones where normal blood cells form.
During the aspiration part of this procedure, the doctor cleans and anesthetizes the skin over the thigh and inserts a thin, hollow needle into the bone. The doctor uses a syringe to remove a small amount of fluid from the bone marrow. Next, a biopsy is performed. The doctor inserts a slightly larger needle to take a small sample of bone and bone marrow.
Fine needle aspiration biopsy (FNA)
FAB is a biopsy performed with a thin needle. Due to the small diameter of the needle, the sample will only contain scattered cells from the lymph node.
A fine-needle biopsy is most often used to check for a return of the disease (relapse) and is almost never used for the initial diagnosis of lymphoma.
Lumbar puncture (cerebro-spinal tap)
Sometimes a lumbar puncture is used to determine if the lymphoma has spread to the cerebrospinal fluid. Most types of lymphoma do not spread to it. A doctor will only prescribe this test for patients with certain types of lymphoma or who have symptoms that indicate the cancer has spread to the brain.
For this procedure, the doctor inserts a thin needle into the lower back after this area has been set under local anesthesia. The doctor then uses a small needle to take a sample of the fluid, which will be sent to a lab for analysis.
A lumbar puncture can also be used to inject a small amount of chemotherapy directly into an area where cerebrospinal fluid circulates.
Collection of pleural or peritoneal fluid
This procedure is used to find out if the lymphoma has spread to the chest or abdomen, where it can cause fluid to build up.
For this procedure, the doctor sets the skin under local anesthesia, inserts a small needle, and uses a syringe to remove a sample of fluid for laboratory analysis. The fluid is called pleural if it is inside the chest, and peritoneal if it is inside the abdomen.
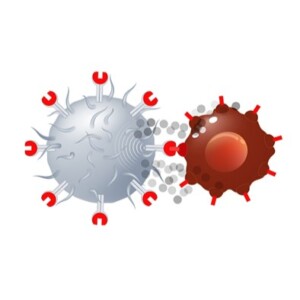
- Blood tests
Doctors take a patient’s blood for tests to measure the number of different types of cells – red blood cells, lymphocytes, white blood cells, and platelets. This information helps determine how advanced the lymphoma is and whether the patient will be able to tolerate certain treatments.
- Visual tests
The oncologist needs the results of imaging tests to find areas of the body where cancer may develop, to find out how widely metastases have spread. In the process of treatment, this is how they check how well the therapy works, which allows to make timely adjustments. Most of these tests are painless and do not require anesthesia.
In Israel, these hardware studies are carried out for lymphoma:
X-rays
When realizing X-rays, radiation to take pictures of areas inside the body is used. The dose of radiation used in most diagnostic tests is so low that it poses no risk to the patient. Findings on a chest X-ray can indicate whether the disease is invasive (large tumors or lymph nodes are usually resistant to conventional therapy).
Computed tomography (CT scan)
A CT scan takes X-rays of the body from different angles. The computer combines images taken from different angles to get a detailed picture of the organs inside the body. Patients with lymphoma often have CT scans of the neck, chest, abdomen, and pelvis. This shows how many lymph nodes are affected, how large they are, and whether the internal organs are damaged by the cancer.
Before the CT scan, the patient may be asked to drink contrast fluid or receive an intravenous injection of a contrast agent. This will give a clearer visualization of the anomalous areas.

Magnetic resonance imaging (MRI)
Like a CT scan, an MRI takes images of the body from different angles. But an MRI machine doesn’t produce X-rays like a CT scan. Instead, it uses magnetic and radio frequency waves.
MRI can provide important information about tissues and organs, especially the nervous system, that cannot be obtained with other imaging modalities. Because this testing method works well for clear images of the bones, brain, and spinal cord, an MRI may be prescribed if the doctor wants to see if the lymphoma has spread to these areas. Diagnosis of lymphoma in Israel is carried out using the 3-Tesla MRI unit, which can detect even the smallest metastases up to 2 mm.
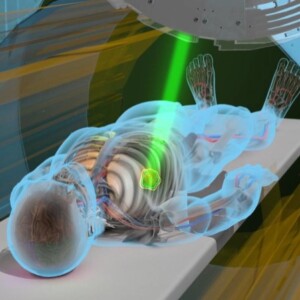
Positron emission tomography (PET scan)
For PET, radioactive fluorodeoxyglucose (a type of sugar) is first injected into the body. A positron camera is then used to detect radioactivity and take cross-sectional images of the body.
PET scan helps determine the extent to which the disease is present and how well the lymphoma is responding to treatment. While a CT scan shows the size of a lymph node, a PET scan shows activity. Israeli doctors conduct tests on a modern device of combined CT and PET systems, which is called PET-CT. Accurate diagnosis on PET-CT allows regular and demonstrative examinations to be carried out without harm to the patient’s body.
Multi-Gated Acquisition (MUGA Scan)
MUGA scan is an imaging test that assesses how well the heart muscle works. MUGA is done to test whether a patient’s body can withstand treatment with certain anti-lymphoma drugs, which in rare cases can damage the heart. Multi-Gated Acquisition can be performed even when patients are resting.
A two-dimensional echocardiogram (ECHO) is sometimes used instead of the MUGA scan to check heart function.
Function tests of lung
Lung function tests are done to assess whether a patient can tolerate certain types of lymphoma therapies that can interfere with bronchopulmonary function.
The tests before starting treatment are prescribed by the doctor. Also, lung function tests are carried out during therapy to assess the functioning of the organ.